Hospital Charges
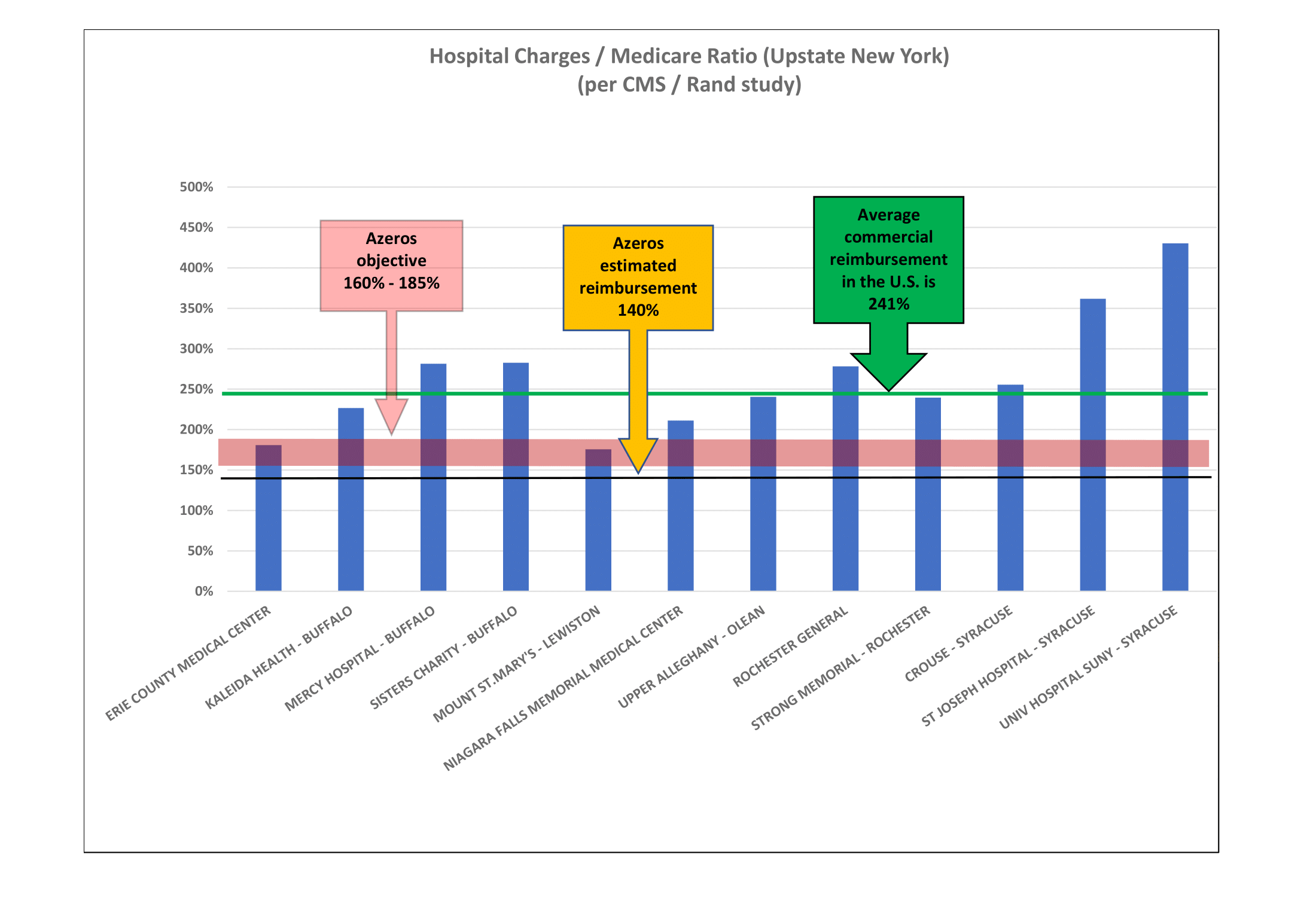
There are no government, competitor, or community influences over hospital billings, resulting in in-patient charges typically ranging from 250% to 400% of Medicare. Few hospitals know their actual cost of rendering a particular patient service or bundle of services, so aggregate revenue objectives drive annual price increases.
Medicare hospital fee allowances are primarily based upon each hospital’s internal operating costs plus a margin. This data is publicly available, from which information Azeros has summarized regional facility charges and relationship to Medicare fees.
Reference Based Pricing
Instead of using hospital charges as a baseline for a payer fee arrangement, Reference Based Pricing (RBP) utilizes Medicare as the baseline, applying a reasonable percentage adjustment factor. RBP factors are determined by Azeros or the self-insured plan. They vary by geography and hospital but are generally in the 150% - 200% of Medicare range. The health plan may also apply the RBP methodology to claims from physicians and ancillary providers. Allowance factors may be lower.
Azeros’ RBP partner offers a Patient Advocacy program that intercedes on behalf of a patient who may be balance-billed by a provider. On behalf of our health plan clients, Azeros’ long-term goal is to bilaterally contract with hospitals at fair reimbursement rates.
Why Don't Insurers Use RBP?
Health insurers are highly unlikely to implement RBP as it would disrupt their favored position with hospitals and lead to billing/payment consistency and transparency.